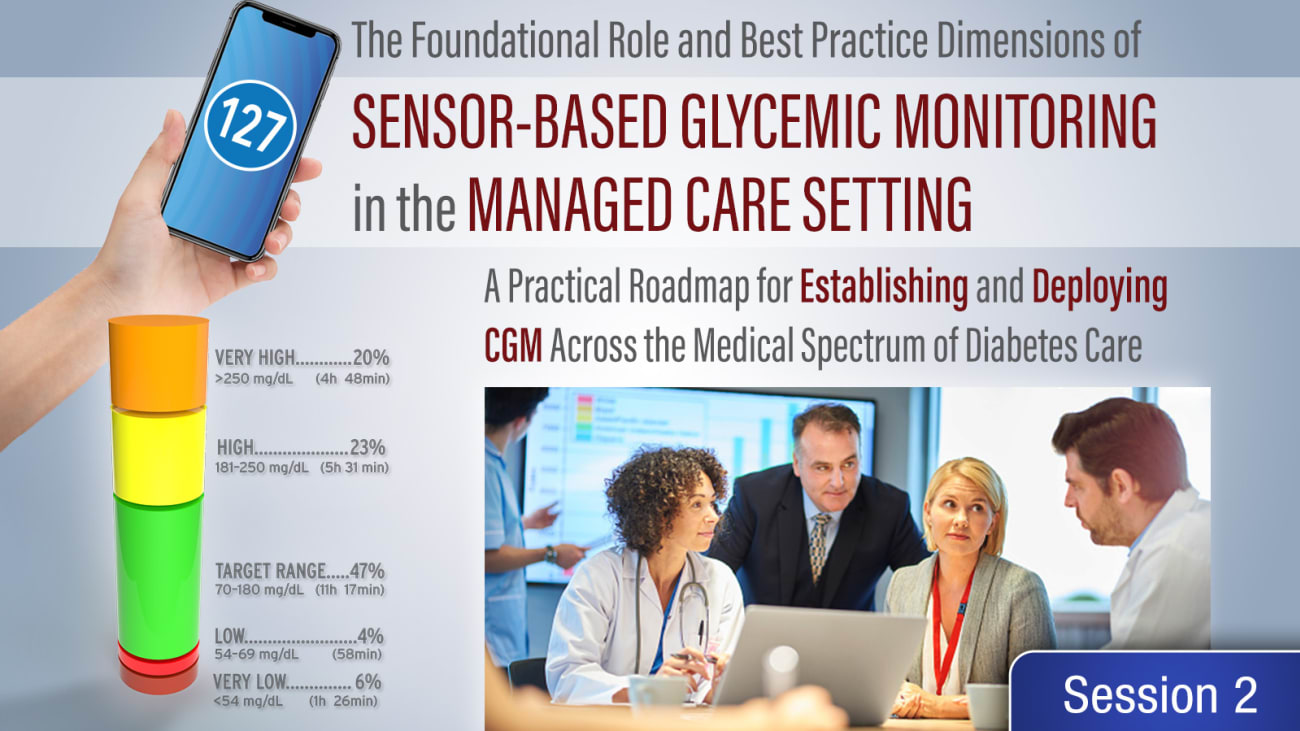
Hello everyone. My name is Earl Hirsch. Coming to you from the university of Washington in Seattle in this I think important part of the program on sensor based glycemic monitoring in the managed care setting. Hopefully you will find this as a practical roadmap road map for establishing and deploying C. G. M. Across the medical spectrum of diabetes care. And I have the privilege of talking to you today about improving overall resource utilization, reducing costs and complications and improving glycemic metrics with sensor based C. G. M. And my hope is is by the end of this presentation you will find the data as compelling as I do that. We need to have greater penetration of this technology in our patients with diabetes. These are my dualities. And let's get started. Our first question to our home monitoring tools, improve outcomes and costs. Well, I always like to look at this from a historical point of view. And if you go back to the 19 twenties thirties and forties, nobody even thought about this. And this was the this was called the Sheftel urine glucose testing kit. It was a chemistry test really from eli lilly. Um very interesting what patients were asked to do back in those days to look at glucose in the urine And then in the 40s and 50 the match in the chemistry test went away and all you had to do was drop a pill in with the you're in glucose urine and the water to show the glucose levels. And then eventually we got into finger stick glucose testing in the 1980s and here we are today with digital readouts of the glucose readings from the meters. And I would ask That during the last years, 100th anniversary of the discovery of insulin, we have data to suggest that these older tools tools had an impact on acute complications and costs actually with the glucose monitors. We did do that to an extent but not to the extent that I think we are or need to now with C. G. M. So let's talk about our newer tools for a moment at least right now. As we speak in the United States, We have four different companies that make see GM technology. And I think the first question if I'm thinking about cost is will see GM reduce visits to the emergency department. And I think this is an interesting study that came out in Jama Network open a couple of years ago looking at the association of multi morbidity, glycemic control and medications with hypoglycemia related E. D. Visits and hospitalizations. It was over 200,000, Almost 202,000 adults with diabetes notice that this was an older population notice that and as expected the vast vast majority of these people had type two diabetes And over 69% of them were either on insulin or so final your areas. And this was looking at this relatively short period of time From the beginning of 2014 To the end of 2016 and what you can see here looking at rates stratified by age and maybe this is not surprising to you. But as the age increases the number of events of hypoglycemia to the increase. And also maybe not surprising to you that we see an opposite sort of graph. When we look at events as it pertains to household income. The greater the household income, the less likely one was going to end up in the E. D. From hypoglycemia. But I think this one is more important and also why we see so much more hypoglycemia with the elderly. As one gets older one has more more comorbidities and the greater the comorbidities. The greater the risk of ending up in the from hypoglycemia. This graph is really interesting to me and it's interesting because we see this J shaped graph in so many different things that we do in diabetes. We are now looking at a hemoglobin a. one c. And the risk of ending up in the E. D. With hypoglycemia. And as you can see and we have shown this Both in type two and type one diabetes, The higher the a. one c. The greater the risk of showing up. And there are a lot of reasons for this. My very simplistic reason. One of my reasons is somebody is checking their blood sugar intermittently. They see a high number they take an extra dose of insulin. It's often too big of a dose. They don't check again and they end up with a severe hypo episode. Not surprisingly. As the A. One CS get very low. We see more hypoglycemia. The lowest risk is actually here. The bottom with a one sees a 5.7- 6.4. I want to point out with these very very low a. one CS. These are often patients with renal disease and renal disease will falsely low the hemoglobin A one C. With the anemia of chronic renal disease. As it turned out having type one diabetes resulted in a 34% increased risk of hypoglycemia related E. D. Visits or hospitalizations. The point is this is a huge societal problem. It's a public health problem. And this is hypoglycemia insulin. And so follow your ears looking at the annual cost of health care resource used from hypoglycemia. This is a busy slide. But what you can see is that with no hypoglycemia costs are the least with severe hypoglycemia. You have the greatest cost. Now these are 200 2000 and 13 the year 2000 and $13. But what you see is the greatest cost over $15,000 is with severe hypoglycemia. Looking at all of the severe hypoglycemia that is seen. This is an expensive adverse event of diabetes therapy mostly was sent with insulin but also with so final your ears. So that's hypoglycemia cost. What about vodka and hyper glycemic emergency. Well this was published relatively recently and it's the last data we have. This comes from the CDC and we're looking both at the E. D. Visits for keto acidosis and inpatient visits for keto acidosis. And you can see these curves are going in the wrong direction from 2009, 2015, 2009, as you will see, turns out to be an important year. Everything seems to be going the wrong way starting in 2009. And what my question really is with this is what happened during Covid anecdotally. We saw so much keto acidosis during Covid partly related to the Covid itself. But I suspect we are going to see much greater numbers of vodka after March of 2020. Now these are data from Jama in 2019. And remember I said that 2009 turned out to be an important year. And we're just going to look at hyperglycemia for a moment. And what we are looking at is hospitalization for hyperglycemia. In this dark line here at the top. And what you see is is that after 2009 hospitalization for hyperglycemia in this youngest age group went up as it turned out the trend also goes up for this dark line in the 45 to 64 year old age group. It did not go up for hyperglycemia In our population over the age of 65. And we have to suspect that a lot of this of course is type one diabetes in this lower age group. But overall when we look at everybody between 2009 and 2015 hyper glycemic crisis increased By 81%. Again a tremendous cost to the system. Now the good news is the length of stay went down. The bad news is cost rose. When we look at this um hypoglycemic crisis and specifically D. K. A. You can see in the blue the length of stay actually went from about 3.5 days down to just a little bit over three days. So the length of stay went down. But the cost went up. In fact The cost of one d. K. A. Was Over $26,000 per episode. $26,000. And that was in 2014. So this is expensive and you and I and everybody knows the cost of a DK episode is much higher. Now In 2022 these are the number of people. So the number went up. The length of stay went down cost went up. So Let's do the math and we can convert this to $2020. Even though this was done six years before that Because in 2014 If you do the math, the number of admissions and the cost per admission were over $5 billion. Now what I did was I went to this medical inflation calculator there are different inflation calculators. I like tom's I don't know who tom is but I use his inflation calculator all the time. And if you do the math with his calculator Comes up to 6.05 billion dollars billion dollars for DK in 2020. The number of cases in the US costs. Well, in excess of six billion in 2022, there's more DK and I actually think this number is going to be much, much bigger. Not only because of the inflation because of what we have seen with covid and how much this is going to rise. Time will tell. Now we all agree DK is expensive. Now the big question is can continuous glucose monitoring, reduce the cost. Was that this was one of the first studies looking at use of freestyle library. One of the sea gMS use in the UK. Over 2400 people with type one diabetes, 30 hospitals in the UK, they were relatively young, more than half women Diabetes duration. 14 years. Non obese not uncommon with type one diabetes. The hospital admission for hyperglycemia and DK was reduced from five to 1% Over this six month period. Now that's an 80% reduction by using the freestyle re break. Now that seems like a huge reduction. But that's just one study, let's look at another population as it turns out it's another population from the UK. And as it turns out they're also using freestyle library. But this was a prospective observational study Again, type one with 900 patients using library, they were a little bit older than the last population, a little bit longer duration of diabetes. But here DK was reduced from 10 to 2 episodes in the six months following initiation of the library. An 80% reduction. Now, how often do you have two different studies giving you the exact exact same result? I mean exactly the same. So there's a signal here and it's a signal that I don't think can be ignored. Okay, so we have two studies with the exact same result. What if we reduce the DK costs in the us by 80 In $2020? Well, we already said It was 6.5 billion. And if we reduce this by 80%,, what we will do is save 4.84 billion dollars. If you do the math, 80% reduction in D. K. I mean these are these are numbers that I can't even fathom. Um there are just too many zeros after the decimal point. That's the cost saving by using the C. G. M. Okay, what about if we now move from the UK to France Real world experience? It's called the relief study. It was published last year Here. It was over 74,000 people with either type one or Type two diabetes. Again initiating freestyle vibrate in the french national claims database. We have type one diabetes and type two diabetes. After 12 months. Look at the glycemic emergencies. If we look at deka, The reduction was 56%,, interestingly. There was no change in glycemic emergencies with hypoglycemia. There was with coma, nothing with hyperglycemia. Overall acute emergencies in type one was reduced by 49%. What's interesting is that even though the numbers were not as large, we saw similar types of decreases 52% for DK with type two We don't know how many were on SGL T two inhibitors. Almost 11% for hypoglycemia. Almost 32% for Coma. 26.5% for hyperglycemia. Now these numbers are low. Nevertheless, For glycemic emergencies it was a 39.4 reduction with the use of freestyle libre In type two diabetes. Again we're getting the same sort of signal when you use this technology acute glycemic emergencies both on the high side and the low side are reduced. Now what they also did, which to me makes complete sense. And in fact our Medicare uh rules for use of C. G. M. Have taken this away and that is was there any difference in reduction in hospitalizations for a glycemic emergency If they were testing zero times a day Or more than five times per day. And as it turns out you had benefit no matter how much they were testing at home with intermittent finger stick testing when they moved then to see gm. Everybody gets a benefit. It doesn't matter what they are doing. And I think there was enough data produce from the Medicare point of view that they took this requirement away. And now when we prescribe N. E C G. M for Medicare beneficiaries, how much they are testing at home. Actually doesn't matter. As you can see from this very large study in France. It didn't matter here. So let's again translate this 54% reduction we saw in France with D. K. To the U. S. Now if we do the math here, we're going to save 3.25 Billion dollars. Now this was not the 80% reduction seen in the UKK but this was a larger population in France. It's still a lot of money and you can quibble which one is more accurate. I I don't think when we're dealing with these numbers, you're saving a lot of money, okay? Can see GM improve outcomes and costs. Let's now move to the US. This was a study published last year by Richburg install is the first author. I was the senior author on this study. We defined acute diabetes events as a combination of inpatient and emergency outpatient events including hyper and hypoglycemia. D. K. A. Hypoglycemic coma coma and hyper osmolarity secondary events was all cause inpatient hospitalization. We looked at over 2400 people and this study was specifically Type two diabetes receiving multiple daily injections before and six months after starting freestyle libre. So before and six months after. This is just. MD multiple injections and type two. This was not for the most part a Medicare age group. The mean age was 54 years. Now. When we look at the actual data. And even as I'm showing you the data right now, I sort of get chills. I always get chills when I show acute diabetes events in patients or outpatient emergency. The blue line is the pre acquisition. The red line is what happened with these acute events after receiving the library. The hazard ratio is .39. The risk reduction is 61 at six months. And we don't usually see these types of hazard ratios. Um in any kind of analysis, let alone a real world study. This was obviously very statistically significant for acute diabetes events and when we look at hospitalizations we see the same thing. The hazard ratio was not as great, but it was still very significant. We still see a risk reduction of all cause inpatient hospitalizations of 32%. And what's interesting about both of these lines is that both of these lines start to separate very soon after starting the C. G. M. Analogy starts right away. So we concluded that these findings provide support for the use of C. G. M. In type two diabetes patients treated with short or rapid acting insulin therapy to improve clinical outcomes and potentially reduce costs. I think the signal here is quite clear. Now there are two types of c. g. m. And we all have our favorites. But it really doesn't matter when you look at which one is better for which patient. I think the more important issue is what happens when we look at the C. G. M. And real world experience. This was an IBM market scan research database. This was another study I was involved with. It is now online. American Journal of american. American Journal of Medicine. Open access. We looked at both decks calm and freestyle libre. In this study we looked at over 3500 people with type one diabetes on dex calm. Excuse me. 3500 patients with type one diabetes more on library than on dex calm. And almost 4000 with type two diabetes. Again more on library than on Dex Calm. But everybody was using multiple injections, basil, insulin and bolus insulin. And what we did was since the numbers were different, we used propensity score matching on everything from demographics provider visits comorbidities, insulin pump use and baseline events. I have learned a lot about propensity score matching and it's away to normalize to populations so you can compare them and that's exactly what we did. It's a it's a statistical tool that the bio statisticians like to use a lot because just like you see here with the number of people on decks common library, both for type one and type two not to mention socioeconomic status, other comorbidities and so forth. This is a tool propensity score matching that allows us to compare these populations. If we start looking at type one diabetes all cause hospitalizations and acute diabetes events with the pink dex calm. The blue library. What you see is these lines are right on top of each other. That the time from C. G. M. Acquisition as far as C. G. M. Acquisition see GM hospitalizations, there was no difference and all cause hospitalizations or acute diabetes events. The p levels were not significant in both. By the same token, there was no difference in type one diabetes with acute hypoglycemic events Or acute hypoglycemic events in type one diabetes. Both of these devices were working the same for this outcome. Now we have Less event less events in type two diabetes. So the confidence intervals are wider. Nevertheless, when we look at all costs hospitalizations and acute events and type two diabetes the lines are on top of each other. There is no difference statistically and the same is true with hypoglycemic events and hypoglycemic events. There was no difference in this real world analysis. So we concluded that patients with either type one or type two diabetes experienced similar reductions of acute diabetes events and all costs hospitalizations when using either brand of C. G. M. X. Com or the freestyle libre from Abbott. So the last point see GM also impacts cost of long term complications. I mean what you can do in these types of studies has looked at trips to the emergency room visits to the hospital. But what the Canadians recently published in 2021 is modeling this so you can look at lifetime costs and what they showed when looking at the lifetime costs in Canadian dollars. This is the direct costs of the C. G. M. North of 30,000 dollars lifetime. But there was this small reduction of cardiovascular disease, A bigger reduction of $15,000 of renal disease, a reduction of ulster amputation, i complications and severe hypoglycemia. And what We were told by these economists is that the willingness to pay in Canada based on a $50,000 quality adjusted life year was close to a was close to 100 that this is a cost effective technology to use two improve all of these long term events. Okay, now here's a study that was published just last week. It wasn't even published. It was presented and that's actually important. This has not been peer review for publication yet. The name of the study is Flash UK. He was presented at diabetes UK on March 30, It was 141 people with type one diabetes And just looking at a one C baseline is blue Oranges at six months. What you see here is a small decrease with the B. G. M. Group. It was 8.5 to 8.2 using finger sticks. But this is what happens with freestyle liberate. It went from 8.7 two, Now that turns out to be a major reduction And Hemoglobin A one C. The difference between the two groups over six months was highly significant. If we look at time and range time and range, we define as a glucose of 70-1, there was no difference in the time and range with fingers to glucose. Testing Time and range. Using freestyle libre improved by 10 From 42% to 52%. That is on average about 2.5 hours a day with greater time and range. And again, this was very statistically significant. There was also a significant reduction in hypoglycemia, interestingly, People were five times more likely for a .5% reduction in a one c. If they were on the library and the incremental incremental costs of $6,800. Now this was converted $2 per quality adjusted life here. And the willingness to pay threshold by the UK by Nice. Now, Nice is the National Institute for Health Care and Excellence. They will pay for things If it's $26,271 per quality. Well, this turned out based on the data, I just showed you To be well under that at only 60 800 dollars for quality And and people argue that this number is too low. And we generally pay in the us for things between 50 $100,000. Well they only paid at $26,000, but this was only $6800. And and so the quotes that came out of this meeting where this was presented and I was not at the meeting in the UK. But the quotes were, everybody with type one diabetes has to be using this technology because this is so overwhelmingly cost effective with everybody willing to pay in the UK for this technology. So I would like to conclude that acute diabetes emergencies are increasing in the US. And I think it's actually worse than the data we have based on what we have seen with covid data continues to accumulate from around the world that C. G. M. Reduces the incidence of these life threatening events. And I have to point out the data is consistent and it's compelling and it's not always exactly the same, but it's always in the right direction and what we saw with amount of money we save and these p levels when the statistical analysis is statistical analyses are done are the same in terms of how convincing, at least it is to me See, GM also appears to be cost effective for chronic complications in type one diabetes. That's very new data we've known about this, but now we have the modeling to show it more formal cost effectiveness. Studies assessing the impact of this technology in different countries are now needed. Because what is cost effective in one country may not always be cost effective in another, due to the fact that the costs are different for the technology itself, for what it costs to treat complications, both acute and chronic and so forth. So this is where I am coming from. This is a University of Seattle here, husky Stadium, The great place, The greatest place to watch college football in the United States. I hope you found this discussion interesting. I know I did, and I want to thank you for your attention.
Related Presenters